Practitioners should stop focusing on “relapse” in substance use disorder and more on recovery.
Written by Amanda Brooks, LCSW, CADC Owner, Brooks Integrated Health Solutions

How would you feel if someone told you that your cancer diagnosis is a result of your moral failings? Or that you have diabetes because you lack the willpower to stop eating cake? Imagine having a dunce cap placed upon your head while treatment professionals encourage your fellow patients to publicly shame you because you had as asthma relapse. Or if the largest treatment facility for your heart failure was jail. Each of us would balk at the audacity of these claims. We would be horrified by the callousness and inhumanity of what has just been described. Yet, this is the reality for people with substance use disorder (SUD).
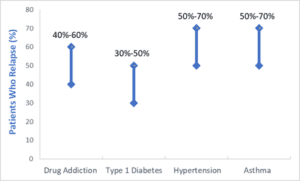
Would you be surprised to learn that relapse rates for SUD are the same, if not better, than common chronic diseases like diabetes, asthma, and hypertension? It’s a shocking reality when a common theme amongst non-addiction treatment professionals is “treatment doesn’t work.” But the evidence is clear; relapse is common for all chronic diseases, including addiction. (1)
So, if it’s not a moral failing, or a lack of willpower…if addiction is a chronic disease just like diabetes or hypertension, what does that mean for treatment that has historically focused on the punitive response to a person’s lack of character? Our understanding of addiction as a chronic disease comprised of biological, psychological, and social contributors has inherently changed the way we treat addiction. No longer seeing addiction as a moral or value focused failing has allowed treatment to move out of, and beyond, acute care settings, and into long-term disease management and monitoring settings, like primary care. By incorporating SUD treatment into whole-person care settings, patients can receive chronic disease management from a team that can address their complex medical history. This harm reduction approach allows providers to leverage the patient/provider relationship to increase motivation for change, while seeing patients for who they are…complex and fascinating humans with differing life experiences. These are individuals, who with compassion and empathy, are capable of change, and deserving of care, like any other person suffering from disease.
Sources
- McLellan, A. T., Starrels, J. L., Tai, B., Gordon, A. J., Brown, R., Ghitza, U., Gourevitch, M., Stein, J., Oros, M., Horton, T., Lindblad, R., & McNeely, J. (2014). Can substance use disorders be managed using the chronic care model? Review and recommendations from a NIDA Consensus Group. Public Health Reviews, 35(8). https://doi.org/10.1007/BF03391707

